 This is a continuation of my discussion of this most important topic from my last blog post titled, “ANESTHESIA MALPRACTICE ~ The Deviation in the Standard of Anesthetic Care During Intubation Resulting in Aspiration ~ part one,” whereby I am setting forth some important questions that need to be answered and why these questions are important when faced with a Medical Malpractice Case involving whether or not there was a breach, or deviation, in the standard of care during an intubation that resulted in an aspiration. The important questions are continued as follows:
This is a continuation of my discussion of this most important topic from my last blog post titled, “ANESTHESIA MALPRACTICE ~ The Deviation in the Standard of Anesthetic Care During Intubation Resulting in Aspiration ~ part one,” whereby I am setting forth some important questions that need to be answered and why these questions are important when faced with a Medical Malpractice Case involving whether or not there was a breach, or deviation, in the standard of care during an intubation that resulted in an aspiration. The important questions are continued as follows:
5.) Prior to Intubation, was it checked whether or not the Patient had Dentures and were the Dentures Removed?
Why is this important? It is vitally important to identify any anatomical abnormality which could not be favorable for a successful intubation of ventilation.
6.) What, if any, measures were taken to make sure that there were no head and/or spinal cord injuries before positioning the head for Intubation?
Why is this important? When performing an intubation on an adult, there is usually a pad or pillow that is positioned under the occiput so that the head is elevated. This will also make sure that the laryngeal, pharyngeal, and the oral structures are aligned.
7.) Was a Rigid Intubation Fiberscope in Use?
Why is this important? In patients where the airway is difficult, a Rigid Intubation Fibroscopes can improve the view of larynx.
8.) Prior to the Intubation was the Patient Provided Pre-Oxygenation?
Why is this important? If intubation proves to be difficult, during the period of apnea and before the tracheal intubation Pre-oxygenation can prevent hypoxia.
9.) During Intubation, was the Sellick’s maneuver performed?
Why is this important? Used successfully and routinely, the Sellick maneuver is used to protect patients during endotracheal intubation from esophageal aspiration and gastric insufflation from positive pressure ventilation.
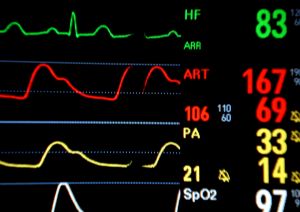
10.) During Intubation, which, if any, of the Following Basic Physiologic Monitors were Performed?
Why is this important? It is imperative that the following physiologic monitors, that are basic, must be in place prior to the induction of anesthesia and tracheal intubation in the emergency department: 1.) Electrocardiography; 2.) Blood pressure that is not invasive; 3.) Pulse oximetry; 4.) End-tidal carbon dioxide analysis; and 5.) Temperature monitoring.
11.) During Intubation, was an End-Tidal/CO2 Detection device (Capnography) Used?
Why is this important? To provide a dynamic and continuous assessment of the ventilatory status of a patient, capnography is used to verify endotracheal tube placement and also the continuous monitoring of the position of the tube.
12.) To Confirm the Placement of the Endotracheal Tube what Method was Used?
Why is this important? If the tube is not positioned correctly in any way there can be adverse and serious consequences and outcomes so the rapid confirmation of the correct tube placement is imperative.
13.) Did the Patient have any Avulsed Teeth and, if so, were the Avulsed Teeth Removed After Intubation?
Why is this important? When a laryngoscope is used, the main injury that is associated with said use is damage to the teeth.
14.) Were, and How, the Endotracheal Tube Cuff Pressures Maintained?
Why is this important? It is very important that the cuff pressure are maintained appropriately by the continuous aspiration of sublottic secretions (CASS) since any leakage around the endotracheal tube cuff can enable pooled secretions and bacteria to enter the trachea that can lead to ventilator associated pneumonia.
15.) Was a Post Intubation Chest Radiograph Obtained?
Why is this important? A chest radiograph is the gold standard currently to confirm the position of a tube.
16.) Did the Patient Exhibit Any of the Following Symptoms?
Why is this important? If the Patient exhibited cyanosis, tachycardia, and/or bronchospasm, this usually indicates an aspiration and within minutes of pulmonary aspiration there is exudation of fluid that neutralizes the aspirate. The second phase involves development of acute lung injury (ALI) which may lead to frank respiratory distress syndrome.
17.) To Rule Out Aspiration, Were Radiological Investigations Ordered?
Why is this important? Within just a few hours, radiographic changes may be visible.
18.) Which, if any, of the Following Treatment Measures were Initiated?
Why is this important? Suggested initial management of aspiration during anesthesia involves positioning the patient and clearing the airway of debris with suctioning. The patient must receive aggressive suctioning of the tracheobronchial tree before using 100% O2. A bronchoscopy may be useful to check for residual debris and remove larger aspirated particles. When deciding whether to treat patients who have aspirated with antibiotics, it is crucial to make the differential diagnosis of pneumonitis from pneumonia. All efforts need to be made to avoid use of empirical antibiotics, and treatment must not be initiated until there is a clear diagnosis of pneumonia.
19.) Did the Clinician Record and Document the Intubation?
Why is this important? It is mandatory that there be a detailed documentation of events in the patient’s medical record.
If you or a loved one has been involved in a Medical Malpractice Case of any type then we are truly sorry. In Medical Malpractice Cases there are strict guidelines so it is very important that you contact us right away so that we may begin to prepare your case so that your case will end with a result that gives you all of the just compensation that is deserving in your particular circumstances.
We may be contacted by phone at (770) 865-8654 , (813) 363-6664; by email at juliericelaw@outlook.com; and/or Contact Us on our website or on the Contact Form on this blog. We are available 24/7 and we look forward to assisting you with your case. All of our legal consultations are free of charge.